The first cases of COVID-19 were detected in Cameroon in early March. How has the situation developed in the region and in Cameroon five months after the start of the pandemic?

The situation today across Africa is, in general, far from the catastrophe that was expected. Africa has about 17 per cent of the world's population, but accounts for only three per cent of recorded COVID-19 cases and only one per cent of deaths. While we must remain cautious about the future evolution of the pandemic, at present the forecasts that were initially put forward have not come true.
We have now entered a phase of increased and sustained transmission among the general population, which could be described as the 'normalisation' of the pandemic. This means that we will have to deal with COVID-19 for some time to come. We need to give ourselves the means to do so in the longer term, to return our societies and economies to a semblance of normality. However, this will only be possible with the arrival of an effective treatment and/or a vaccine that is accessible, available and affordable to all African countries. Any treatment or vaccine must be adapted to the specific conditions in each context, to provide practical solutions, for instance regarding any issues of cold chains, medical protocols, etc.

However, with the national health system’s staff and material resources depleted or redirected towards COVID-19, we are now facing another epidemiological risk from diseases such as cholera and measles which are endemic in Cameroon. It’s crucial we ensure the continuity of care for communities and patients affected by these diseases through integrating the pandemic response into the regular health system. That is why, in particular, specialised health centres, dedicated to COVID-19 care, have been set up to enable other hospitals to continue responding to other epidemics and diseases, instead of being overwhelmed by COVID-19 care.
What is the role of epidemiology in such a situation and how do we analyse the epidemic today?
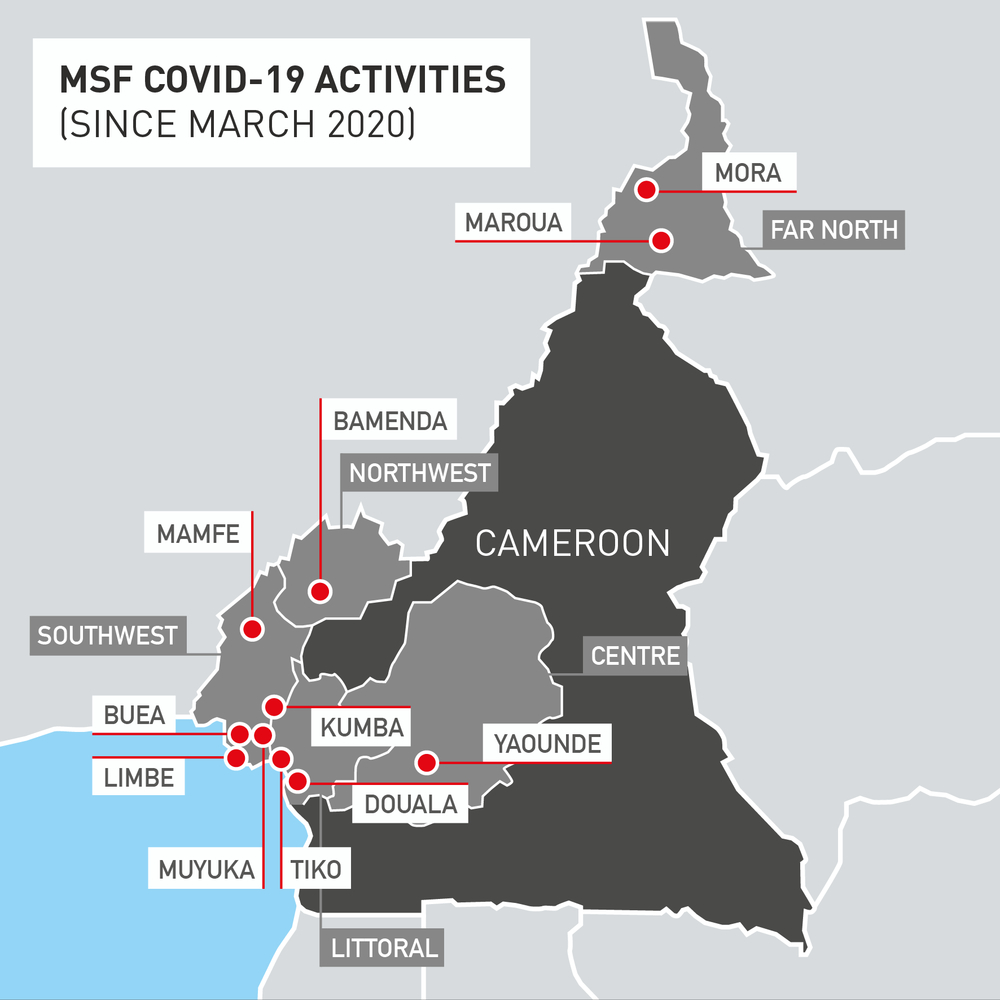
At the start of August, we launched community activities in Cité Verte, one of the three most affected districts in the Central region. We’ve seen that fewer people are coming to hospitals at the moment, so we need to ensure they have easy access to care, even at local healthcare centres within the communities. To do so, we are now running community information sessions, as well as follow-up home visits for moderate confirmed cases and referels for the most severe patients to the dedicated hospital. We are also supporting patient tracing and epidemiological surveillance, as it is epidemiology that allows us to have this information and to guide our work.
Franck Ale – The role of the epidemiologist is to track cases, and to set up strategies to identify and investigate outbreaks when cases are detected. An important task for epidemiologists during an epidemic is the collection, compilation and analysis of patient medical information, which helps to guide public health activities in areas where there is an outbreak. In doing so, epidemiologists help all those engaged in the fight to take effective action to quickly contain the disease. However, the data available on the current pandemic remains incomplete because of the limited testing capacity and the strategies that have been implemented around the world. For instance, if the countries decide to test extensively or only people entering the country to prevent any imported cases.
Laboratory limitations have always been a problem when trying to trace the spread of a disease. This is common with epidemics, such as measles or cholera, where it is often very difficult to confirm all cases in the laboratory. With the coronavirus pandemic, many countries have tried to increase their testing capacity, particularly by reinforcing laboratory facilities. At the beginning of the outbreak in West Africa, for instance, only Senegal was able to test for coronavirus. Today, almost all countries in the region can identify the virus. Yet they are still limited by their ability to have real-time tests available and to get the necessary supplies.
At the moment, the virological Polymerase Chain Reaction (PCR) test is recommended by the World Health Organization (WHO). This test detects the presence of the genetic material of the coronavirus in samples collected from the nasal system of the patient to confirm whether the virus is still present. The samples are then analysed in highly sophisticated laboratories and results are generally available within 48 hours. Another type of test, the rapid diagnostic test, is used to confirm the presence of the virus antigen or anticorp in the test subject’s nose or blood. With this test, you can get the result faster, in 10 to 15 minutes, on site. The rapid diagnostic test is still being evaluated, as its accuracy is lower than the PCR test.
However, for health workers in the field, the sooner a test result can be confirmed the better, as the goal of a surveillance system is not necessarily to succeed in confirming all cases, but rather to set up a robust system for rapid case identification. Yet, to do so, we need reliable and accessible tools, hence the need to make rapid diagnostic tests available, especially in remote areas outside African capitals.
Evaluations of rapid diagnostic tests have been carried out in Cameroon, can you tell us more about this?
Yap Boum – Different diagnostic tests provide answers to different questions. The first is whether the virus is present in the person who is tested, using either PCR or rapid diagnostic test. The second question is whether the person has been exposed to the disease. Antibodies against COVID-19 are also looked for in the blood of those that are tested, in order to know whether the person has been recently infected by the virus. This allows us to assess the degree of transmission of the virus in the community, which is also another indicator to measure the evolution of an outbreak.
In Cameroon, the team coordinating the national response has decided to use rapid diagnostic tests, even though the test recommended for COVID-19 diagnosis by the WHO remains the virological PCR test. As we need to have faster access to the diagnosis to increase the number of people we can test, Epicentre, MSF and national coordinating team for the response wanted to assess the rapid diagnostic test, in comparison to the PCR test. To that end, Epicentre and MSF worked with the National Health Emergency Operations Centre (COUSP) to set up a project to evaluate the different tests available in screening and healthcare centres. This included the Djoungolo hospital in Yaoundé where MSF cares for patients with COVID-19. Following this study, it has become possible to test in all health districts, while getting a result in a relatively short time. We are now working on a mobile screening strategy, which would allow us to install mobile testing teams in markets, universities and high-traffic areas.
