In April, Médecins Sans Frontières/Doctors Without Borders (MSF) began supporting the national response to the COVID-19 health emergency in Niamey, the epicentre of the COVID-19 pandemic in Niger. MSF teams that regularly work in several other parts of the country have also implemented a number of measures as the pandemic spread to other regions. In a context characterised by stigma and violence, there are many challenges.
After six weeks of construction, the MSF treatment centre for COVID-19 patients at the Amirou Boubacar Diallo National Hospital in Niamey opened its doors. The centre has 50 beds, with the potential to accommodate up to 100 beds in case of a peak in patient numbers. Denis Dupuis, logistics and technical coordinator for MSF, says: "In just a few weeks, we set up a semi-permanent, completely autonomous structure to treat patients and limit the risk of transmission to the neighbouring hospital. The centre has superior infection control conditions. The beds are separated by between one and two metres and the whole space is bright and well-ventilated. All of this will limit the risk of infection and better protect medical staff and patients."
To ensure the smooth running of this facility, MSF recruited and trained more than 100 new members of staff. For example, patients requiring oxygen are jointly treated by MSF and Ministry of Public Health teams.
The centre is divided into five main buildings. One of these receives suspected cases with complications, while the other four are for confirmed cases requiring hospitalisation.
Call centre support and mobile teams

MSF is supporting the Ministry of Health, through the SAMU’s call centre, 24 hours a day, seven days a week, as well as mobile teams in five communes in Niamey. The aim is to improve the identification and follow-up of COVID-19 confirmed patients. [©Nathalie San Gil/MSF]
Beyond the treatment centre, in Niamey, MSF is supporting the Ministry of Public Health emergency medical assistance service call centre, which runs 24 hours a day, seven days a week, and mobile teams that operate in five communes of Niamey. The joint MSF and Ministry of Public Health intervention teams provide technical support in verifying alerts, organising triage and referring serious cases from health centres to the treatment centre. These teams also provide psychological support.
Audace Ntezukobagira, coordinator of the mobile emergency team in the Sahel, explains: "This work within communities is crucial because the response to a pandemic cannot be done only in health centres. It is a commitment we must keep. People are still afraid of being stigmatised by their neighbours if an ambulance with men in protective suits arrives at their homes. A major awareness-raising effort is being carried out to ensure a better understanding of the disease and to ensure solidarity, kindliness and confidence in this response. "
The pandemic brings with it many rumours and a lot of misinformation throughout the country, adding a further layer of complexity. Many people have expressed doubts about the existence of COVID-19. Even today, rumours and speculation are still rife. In such a context, it is not always easy for everyone to comply with preventive measures, which risks fostering new chains of contamination. This is why MSF is working with communities to ensure they have the right information and that everyone feels part of the response.
In other regions
Elsewhere in the country, MSF teams have also put in place measures to protect medical staff, patients and the most vulnerable people. In MSF-supported health facilities, prevention, hygiene and infection control measures have been reinforced, with isolation and patient triage zones in case of a suspected case of COVID-19 set up. In addition, health awareness and promotion activities have been strengthened.
MSF teams are also maintaining active epidemiological surveillance, on COVID-19 and beyond, particularly in anticipation of seasonal peaks in the number of patients with malaria and malnutrition with the onset of the rainy season and the so-called hunger gap, when stocks of the previous harvest are likely to run out.
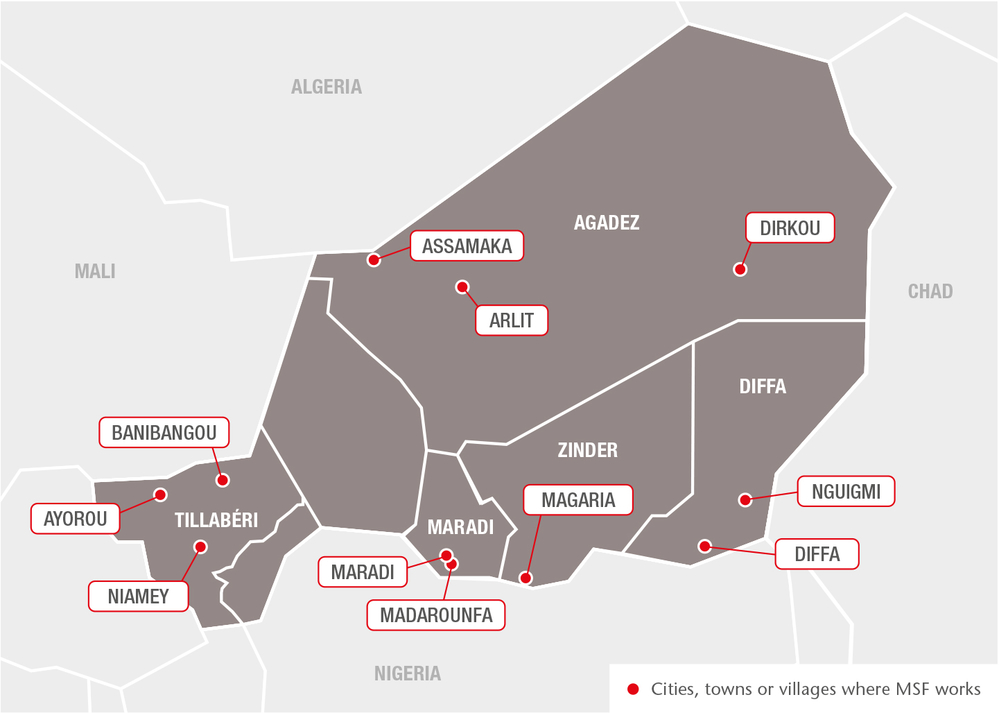
In Zinder, Maradi, Agadez, Diffa and Tillabéry regions, where MSF teams are present, vigilance has been increased following the confirmation of several patients with COVID-19 in most of these areas.
Humanitarian crises don't stop, challenges increase
In the face of the spread of COVID-19, there are many challenges. The first is a global lack of protective equipment, and the difficulty of delivering it to more remote areas.
In some areas, access to communities for humanitarian and medical teams is made even more difficult by insecurity. Armed conflict and violence have not stopped during the pandemic. In the regions of Diffa, in the south-east, and Tillabéry, in the south-west, MSF is particularly concerned about how the new virus could affect people living in precarious environments. Internally displaced people, migrants or refugees, living insecurely in camps, are already very vulnerable. They will be even more exposed to the threat of COVID-19 if they are unable to comply with protective measures, such as hand hygiene, physical distancing or isolating suspected cases, because of their already limited access to healthcare.
In light of all these challenges, it is essential that the Ministry of Public Health and all the humanitarian organisations present in Niger, including MSF, work together in the fight against COVID-19. An increase of the COVID-19 response is needed. However, with the onset of the seasonal peak of malaria and malnutrition, it is also important that health programmes and affordable primary and secondary healthcare services are maintained and delivered in the most appropriate manner, to avoid creating further health emergencies.
MSF has worked in Niger since 1985 and regularly supports the public health system in the management of epidemics in Niger, such as cholera, measles and meningitis. At the moment, MSF teams are also providing free quality medical care to people in the regions of Agadez, Diffa, Tillabéry, Zinder and Maradi. Our objective is always to facilitate access to healthcare for vulnerable people and to guarantee relief to those who need it, regardless of race, religion, and political or other affiliations.
