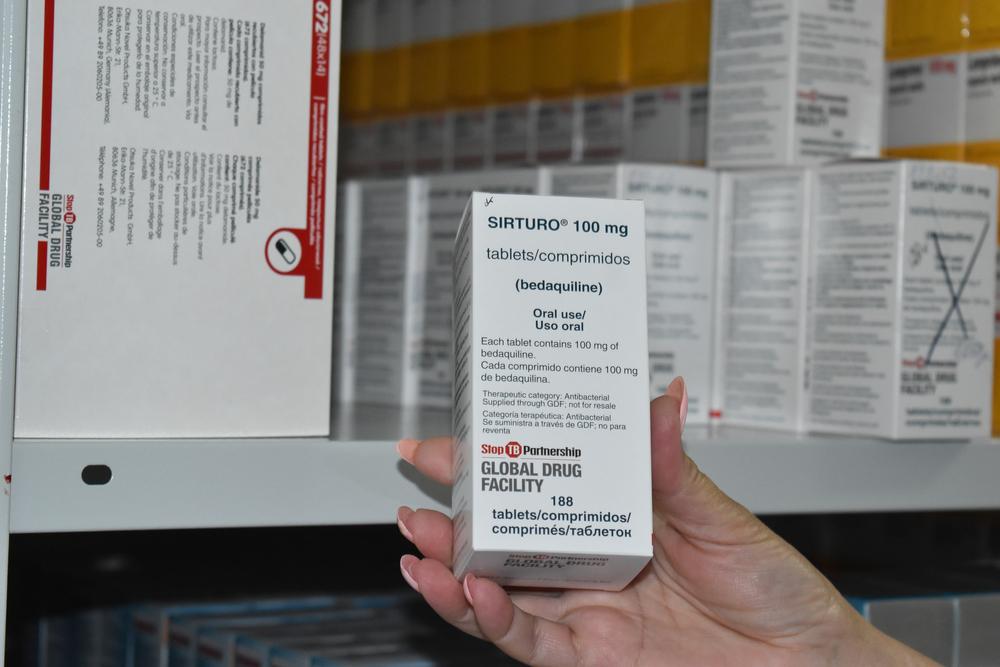
Access to TB drug bedaquiline, a backbone medicine for drug-resistant TB treatment regimens, remains out of reach for too many
Geneva, 26 April 2023 – Ahead of Johnson & Johnson’s (J&J) annual shareholders meeting, the international medical humanitarian organisation Médecins Sans Frontières/Doctors Without Borders (MSF) demanded that the US corporation publicly commit now to not enforce its secondary patents on the tuberculosis (TB) drug bedaquiline in all countries with a high burden of TB, and allow generic manufacturers to supply more affordable, quality-assured generic versions of this lifesaving drug to everyone, everywhere who needs it. Access to affordable generic versions of bedaquiline is presently being blocked by J&J’s secondary patents in at least 25 of the 43 countries with a high burden of TB or drug-resistant TB (DR-TB). With more effective and patient-friendly treatment regimens available for people with DR-TB, there is a need, now more than ever, to accelerate access to affordable treatment and save more lives.
“Back when HIV treatment was first rolled out, competition among generic producers helped lower drug prices and accelerated treatment rollout in many countries,” said Christophe Perrin, TB Pharmacist with MSF’s Access Campaign. “We are deeply concerned that the persistent high price of bedaquiline will continue to block countries from rolling out the newer, shorter, game-changing, all-oral regimens for treating deadly, drug-resistant forms of TB. It is high time that J&J act responsibly by pledging not to enforce secondary patents for bedaquiline, withdrawing all related patent applications, and not pursuing any action against generic manufacturers who could export affordable versions of the drug to high-TB-burden countries where secondary patents remain.”
While J&J’s patent on the base compound of bedaquiline expires in 2023 in most countries, it has resorted to 'patent evergreening' by filing additional patents to extend its monopoly on the drug until 2027 in many high-TB-burden countries. In a landmark decision last month, however, the Indian Patent Office rejected one such evergreening attempt by J&J, by denying the corporation a secondary patent in the country, which would have extended its monopoly for four more years. The ruling was a result of a ‘pre-grant opposition’ filed by two TB survivors—Nandita Venkatesan from India, and Phumeza Tisile from South Africa—who both were forced to endure the older, more toxic DR-TB treatments that lasted up to two years and caused excruciating side effects: they both lost their hearing from the old treatment. As a result of the ruling in India, manufacturers in the country will be able to produce and supply affordable, quality-assured generic versions of bedaquiline once the primary patent expires in July 2023.
Bedaquiline is the backbone of almost all treatment combinations newly recommended by the World Health Organization (WHO) for DR-TB, but currently accounts for 35-40% of the price of shorter, and 35-70% of longer, regimens. It is the main cost driver in the WHO-recommended, 6-month, all-oral BPaLM regimen (comprised of bedaquiline, pretomanid, linezolid and moxifloxacin), with bedaquiline accounting for US$272 out of the total $570 price for the treatment combination. J&J currently prices the drug at $1.50/day for an adult treatment ($272/six months). But with scale-up and generic competition, the price of bedaquiline would be expected to drop, bringing it closer to its target price of $0.50 per day as estimated by researchers.
“The introduction of the new 6-month BPaLM regimen in Sierra Leone has been a groundbreaking milestone,” said Dr Manisha Kumar, MSF Medical Coordinator in Sierra Leone. “Being the first country to routinely offer this shorter and more effective drug-resistant TB treatment outside the setting of a clinical trial is revolutionary, especially considering that many people here struggle to access care due to distance, bad roads and high transportation costs. Adherence to longer treatment regimens and stigma also continue to pose significant challenges. With the lower pill burden and shorter duration of BPaLM, more people with drug-resistant TB can be cured faster and with less suffering.”
TB was the leading infectious disease killer until the COVID pandemic. The number of people newly diagnosed with TB including DR-TB, in 2020 fell by 18% from the previous year due to disruptions to health systems and services caused by the pandemic, with only a partial recovery in 2021. In 2021, only one in three people with DR-TB received treatment for the disease.
“Too many lives have been lost to this killer disease. J&J must give up its secondary patents to make way for the supply of affordable generics. People with TB deserve urgent access to shorter, safer, and affordable treatments,” said Perrin.
MSF is the largest non-governmental provider of TB treatment worldwide and has been involved in TB care for 30 years, often working alongside national health authorities to treat people in a wide variety of settings, including chronic conflict zones, urban slums, prisons, refugee camps, and rural areas. As of September 2021, across 60 programmes in 41 countries, MSF treated 17,000 people with TB, and 2,300 people with DR-TB, including with the newer drugs.