Geneva, 21 December, 2018—The international medical humanitarian organisation Médecins Sans Frontières (MSF) today welcomed new World Health Organization (WHO) treatment guidelines that recommend drug-resistant tuberculosis (DR-TB) be treated with oral drugs only, including newer, more potent drugs with fewer side effects, such as bedaquiline. Two injectable drugs known to cause deafness and other severe side effects are no longer recommended in the new guideline – an important step towards more tolerable treatment for all patients.
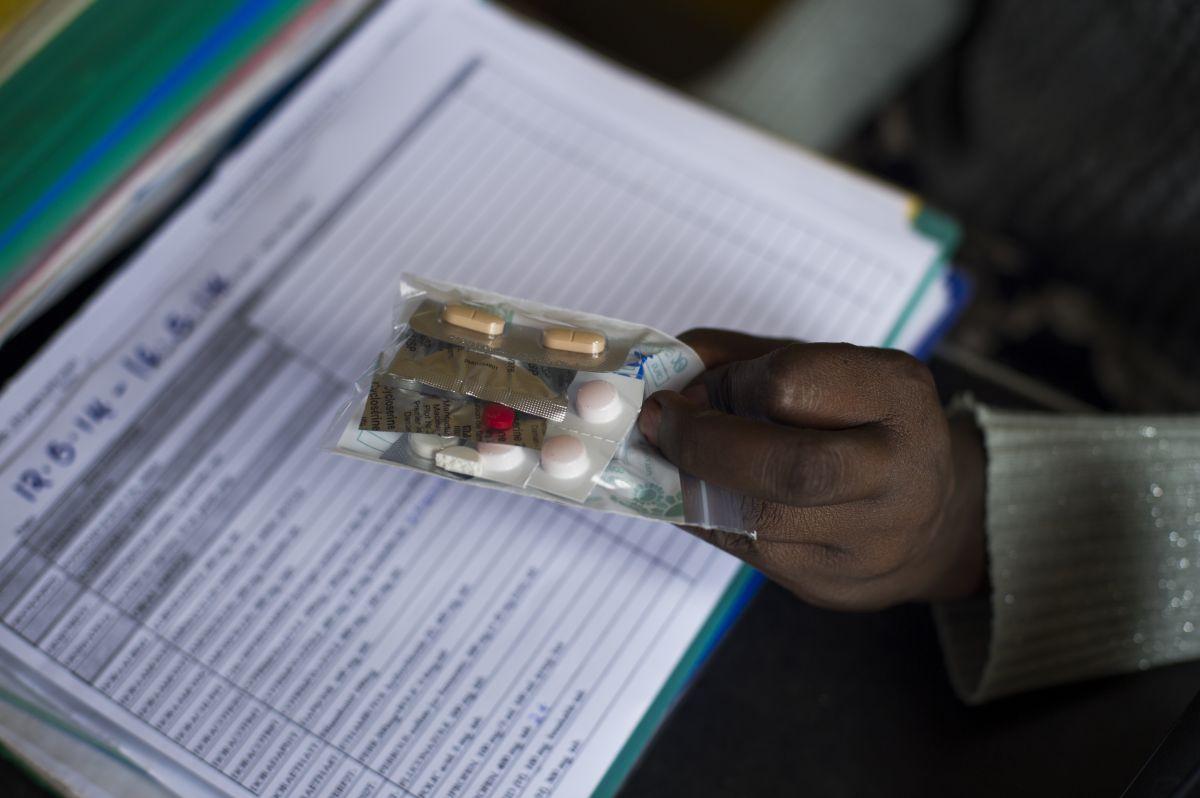
The recommended 18 to 20-month treatment regimen includes more potent drugs – bedaquiline, linezolid, levofloxacin and moxifloxacin – that can help improve cure rates, reduce deaths and cause people far fewer side effects. MSF called on countries with large numbers of people with DR-TB to urgently start implementing these new treatment guidelines for at least half of new DR-TB cases by September 2019, and to make efforts to reach all people in need by March 2020.
“The new WHO recommendations offer the best opportunity in a long time to finally start improving treatment for people with drug-resistant TB, using better drugs that cause fewer debilitating side effects,” said Dr. Naira Khachatryan with MSF in Armenia. “The time is now for countries with large numbers of people with DR-TB to swiftly update their policies and roll out the newer treatment regimen that is more effective and easier for people to tolerate. Let’s not waste a minute in putting an end to the suffering of people who have to endure toxic and agonizing treatment with drugs that must be injected.”
An estimated 558,000 people developed DR-TB in 2017, but only 25% were treated. Standard DR-TB treatment used by most countries up to now has required people to take more than 14,000 pills over a period of nearly two years, including up to eight months of the painful daily injections with severe side effects. Just over half of people are cured.
Findings from an observational study run by MSF and partners following 1,200 people on DR-TB treatment (endTB*) helped to affirm the safety and effectiveness of the newer oral drugs, bedaquiline and delamanid, and supported the WHO’s recommendation that bedaquiline, in particular, be considered a core drug for treatment of MDR-TB. Although insufficient data supports the use of bedaquiline and delamanid for longer than 6 months, or in combination, countries should utilise these drugs beyond six months as needed.
“The recommendation for new all-oral treatment is a critical step in the right direction that will make this arduous treatment more tolerable for people and save more lives,” said Sharonann Lynch, HIV & TB Policy Advisor for MSF’s Access Campaign. “But to really put an end to the high number of senseless deaths caused by this ancient disease, we need even better treatment that can cure TB much faster and reduce the burden on people’s lives.”
The change in treatment guidelines will more than double the number of people with DR-TB for whom treatment with bedaquiline is recommended. MSF, along with other civil society organisations, have been calling on US pharmaceutical corporation Johnson & Johnson (J&J)—today’s only producer of bedaquiline—to cut the price of the drug in half for all developing countries, to $1 per day, so that people who urgently need it can have access to it. J&J received ample taxpayer money for the development of bedaquiline and should in return make this lifesaving drug affordable for all those who need it.