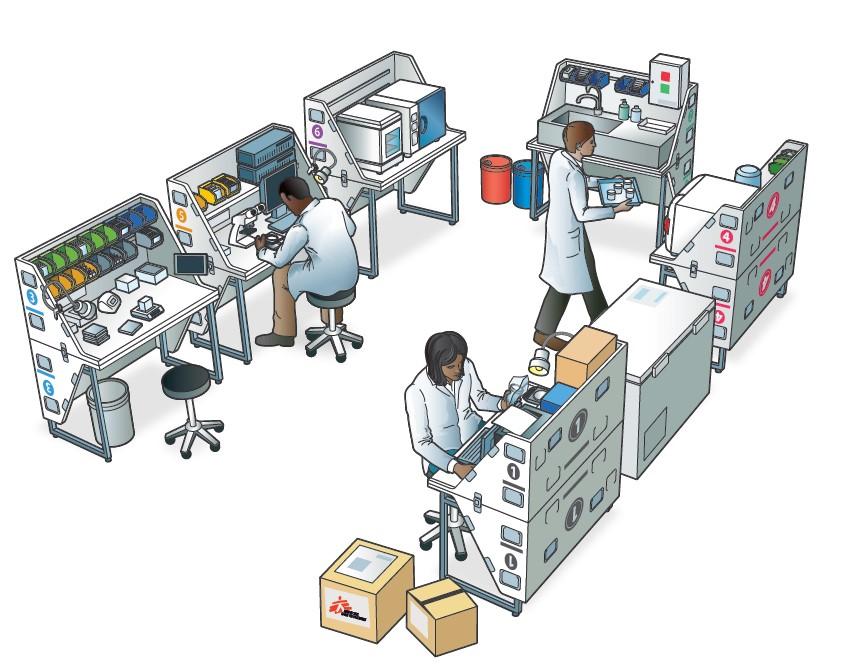
In September 2023, Médecins Sans Frontières/Doctors Without Borders (MSF) launched its ‘Mini-Lab’ initiative in its hospital in Bentiu, Unity State; a transportable, self-contained, quality-assured, microbiology laboratory that aimed to improve diagnosis relevance and treatment effectiveness.
Six months later, Isaac Mumbere, MSF ‘Mini-Lab’ Supervisor shares the achievements of the microbiology lab, both for patients and doctors.

1. How has the microbiology lab improved the quality of care MSF teams deliver in our hospital?
Since last September, the MSF microbiology lab has already shown encouraging results and we have been able to witness the positive impact it has on the medical diagnosis and treatments we provide. Overall, out of the 348 samples that were collected, 39 came back positive and all patients were treated with appropriate antibiotics and clinical care. We identified 11 patients presenting with multidrug-resistant organisms that the medical team also managed to treat rapidly.
Thanks to improved laboratory diagnosis and quick results, clinicians can offer better treatment options, enabling faster recovery and shorter hospital stays for patients, increasing beds availability for other patients in need. The microbiology lab has also helped us detect potential micro-resistant outbreaks and therefore adjust our infection, prevention and control measures in the different wards to prevent further spread of diseases in the hospital.
2. Can you tell us about a patient whose condition was improved thanks to the microbiology lab?
Last November, a one-month-old baby boy, born prematurely in our facility, was admitted for an infection. A blood sample was collected and while waiting for the results, the doctors prescribed broad-spectrum antibiotics. In 48 hours, the microbiology tests revealed that the patient had klebsiella pneumonia, a dangerous infection with a tangible risk of death – especially for patients who have been taking certain antibiotics for a long time. Further tests showed that the young patient was resistant to a wide range of antibiotics, including penicillins, cephalosporins, and monobactam aztreonam, which are among the broad-spectrum antibiotics usually prescribed.
The treatment was adjusted immediately. The baby boy was isolated, treated and after seven days, he was able to go home with his mother. Without the microbiology lab, we would have most likely lost the patient to the infection. MSF ‘Mini-Lab’ helps us reduce neonatal mortality.
3. How has the microbiology lab impacted the collaboration within our teams?
The microbiology lab has significantly eased the medical team's work and made the collaboration with the laboratory team more efficient, directly improving the quality of care for our patients. In the past few months, patients admitted to our neonatal ward were presenting similar symptoms. The medical team requested the lab team to run microbiological tests and the samples revealed the same highly contaminated pathogenic organism. Specific resistance tests later established the presence of multi-drug resistance organisms.
The medical team provided better-targeted treatment to each patient, and we enhanced our infection, prevention and control measures in the hospital. The results provided by the microbiology lab have also increased the teams’ knowledge in managing multi-drug resistance organism
4. After six months, are there any challenges the teams are facing?
Some of the patients who reach our facility have been taking antibiotics at home or other medical facilities for several days. This can affect microbiology diagnosis and we must keep this in mind when providing treatment and continue to closely monitor the conditions of our patients to adjust the treatment if needed.
As the implementation of the ‘Mini-Lab’ is relatively recent, the medical teams are still getting used to the possibility of requesting tests before prescribing antibiotics. It is an ongoing adjustment for everyone, but we regularly conduct awareness sessions with the teams to highlight the improvement the lab can bring.

5. Like MSF ‘Mini-Lab’, how do you think innovation can support healthcare in South Sudan and similar contexts worldwide?
In a lower-resource setting such as South Sudan, surveillance data on antimicrobial resistance are a pressing concern. Data analysis enables us to provide epidemiology indicators for local antimicrobial resistance surveillance, monitor evolutions and predict patterns. Such tools and services support early interventions and improve the quality of care. It directly benefits communities who live in areas that lack functioning facilities and suffer from fragile healthcare systems.



